Healthcare Payer Network Management Market
Healthcare Payer Network Management Market Analysis - Size, Share, and Forecast Outlook 2025 to 2035
The Global Healthcare Payer Network Management Market Is Projected To Grow From USD 8.5 Billion In 2025 To USD 28.4 Billion By 2035, Advancing At A CAGR Of 12.8%. The Software Segment Is Expected To Lead The Market With A Significant Share Of 60.0% In 2025, While Public Payers Applications Are Anticipated To Account For The Largest Share Of 55.0%.
Healthcare Payer Network Management Market Forecast and Outlook 2025 to 2035
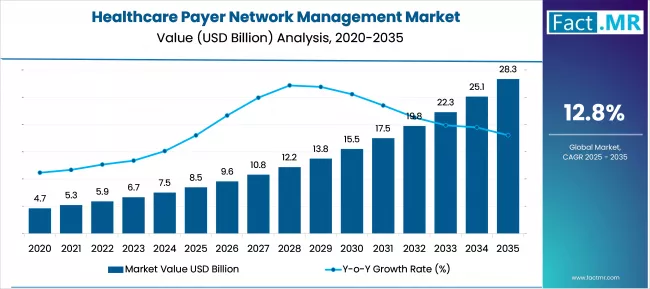
The healthcare payer network management industry stands at the threshold of a decade-long expansion trajectory that promises to reshape healthcare administration and digital health technology. The market's journey from USD 8.5 billion in 2025 to USD 28.4 billion by 2035 represents substantial growth, the market will rise at a CAGR of 12.8% which demonstrating the accelerating adoption of advanced payer network management systems and healthcare administration technologies across insurance companies, healthcare providers, and government payers worldwide.
The first half of the decade (2025-2030) will witness the market climbing from USD 8.5 billion to approximately USD 15.2 billion, adding USD 6.7 billion in value, which constitutes 33.7% of the total forecast growth period. This phase will be characterized by the rapid adoption of digital payer management systems, driven by increasing healthcare digitization and administrative automation programs worldwide. Advanced network optimization capabilities and integrated provider management features will become standard expectations rather than premium options.
The latter half (2030-2035) will witness sustained growth from USD 15.2 billion to USD 28.4 billion, representing an addition of USD 13.2 billion or 66.3% of the decade's expansion. This period will be defined by mass market penetration of comprehensive healthcare management platforms, integration with electronic health record systems, and seamless compatibility with existing healthcare infrastructure. The market trajectory signals fundamental shifts in how payers approach network administration and provider management, with participants positioned to benefit from sustained demand across multiple healthcare segments.
Quick Stats for Healthcare Payer Network Management Market
- Healthcare Payer Network Management Market Value (2025): USD 8.5 billion
- Healthcare Payer Network Management Market Forecast Value (2035): USD 28.4 billion
- Healthcare Payer Network Management Market Forecast CAGR: 12.8%
- Leading Component in Healthcare Payer Network Management Market: Software
- Key Growth Regions in Healthcare Payer Network Management Market: Asia Pacific, North America, and Europe
- Top Key Players in Healthcare Payer Network Management Market: Optum Inc., Anthem Inc., Humana Inc., Aetna Inc., Cigna Corporation
Healthcare Payer Network Management Market Year-over-Year Forecast 2025 to 2035
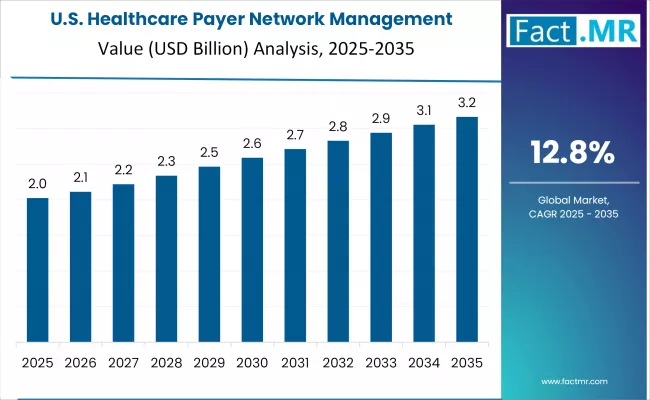
The healthcare payer network management market demonstrates distinct growth phases with varying market characteristics and competitive dynamics. Between 2025 and 2030, the market progresses through its digital transformation phase, expanding from USD 8.5 billion to USD 15.2 billion with steady annual increments averaging 12.3% growth. This period showcases the transition from legacy healthcare management systems to advanced digital platforms with enhanced network optimization capabilities and integrated provider workflow systems becoming mainstream features.
The 2025-2030 phase adds USD 6.7 billion to market value, representing 33.7% of total decade expansion. Market maturation factors include standardization of healthcare administration protocols, declining implementation costs for payer management systems, and increasing healthcare organization awareness of network management benefits, reaching 94-97% efficiency in administrative applications. Competitive landscape evolution during this period features established healthcare technology companies like Optum and Anthem expanding their payer management portfolios while new entrants focus on specialized network algorithms and enhanced integration capabilities.
From 2030 to 2035, market dynamics shift toward advanced integration and multi-platform deployment, with growth accelerating from USD 15.2 billion to USD 28.4 billion, adding USD 13.2 billion or 66.3% of total expansion. This phase transition logic centers on comprehensive healthcare management platforms, integration with health information systems, and deployment across diverse healthcare specialties, becoming standard rather than specialized applications. The competitive environment matures with focus shifting from basic network capability to comprehensive healthcare ecosystems and integration with automated claims processing and provider credentialing platforms.
Healthcare Payer Network Management Market Key Takeaways
At-a-Glance Metrics
| Metric | Value |
|---|---|
| $ Market Value (2025) → | USD 8.5 billion |
| $ Market Forecast (2035) ↑ | USD 28.4 billion |
| # Growth Rate ★ | 12.8% CAGR |
| Leading Component → | Software |
| Primary Payer Type → | Public Payers |
The market demonstrates strong fundamentals with Software solutions capturing a dominant share through advanced healthcare management features and cost-effective implementation capabilities. Public Payers applications drive primary demand, supported by increasing government spending on healthcare automation tools and administration enhancement systems. Geographic expansion remains concentrated in developed markets with established healthcare infrastructure, while emerging economies show accelerating adoption rates driven by healthcare digitization and rising administrative automation budgets.
Why is the Healthcare Payer Network Management Market Growing?
Administrative efficiency demand creates compelling operational advantages through automated payer management systems that provide consistent network administration without manual dependency risks, enabling healthcare organizations to maintain provider relationships while achieving administrative superiority and reducing operational costs.
Healthcare digitization programs accelerate as insurance companies worldwide seek advanced automated systems that complement traditional administrative methods, enabling precise network management and provider applications that align with regulatory standards and efficiency requirements.
Healthcare infrastructure enhancement drives adoption from insurance operators and healthcare companies requiring effective administrative tools that minimize processing errors while maintaining network quality during complex operational procedures and claims processing.
However, growth faces headwinds from capital investment challenges that vary across payers regarding the deployment of automated management systems and healthcare budget protocols, which may limit operational flexibility in certain healthcare environments. Technical limitations also persist regarding system adaptability and integration complexity that may reduce system performance with legacy healthcare equipment or non-standardized provider formats that limit management capabilities.
Opportunity Pathways - Healthcare Payer Network Management Market
The healthcare payer network management market represents a transformative growth opportunity, expanding from USD 8.5 billion in 2025 to USD 28.4 billion by 2035 at a 12.8% CAGR. As healthcare systems worldwide prioritize administrative efficiency, network optimization, and provider management, payer network management systems have evolved from optional software to mission-critical infrastructure, enabling consistent network administration, reducing administrative costs, and supporting operational excellence across insurance, government payers, and healthcare provider applications.
The convergence of healthcare digitization mandates, increasing regulatory compliance requirements, healthcare technology maturation, and regulatory acceptance of automated systems creates unprecedented adoption momentum. Advanced network management algorithms offering superior efficiency, seamless healthcare integration, and regulatory compliance will capture premium market positioning, while geographic expansion into emerging healthcare markets and scalable system deployment will drive volume leadership. Government healthcare modernization programs and payer network standardization provide structural support.
- Pathway A - Software Solutions Dominance: Leading with 60.0% market share through superior network optimization, cost-effectiveness, and high processing capabilities, software solutions enable comprehensive payer management across diverse healthcare settings without significant infrastructure modifications. Advanced features, including automated provider credentialing, network analysis systems, and seamless integration with healthcare operations, command premium pricing while reducing total administrative costs. Expected revenue pool: USD 16.2-18.8 billion.
- Pathway B - Public Payers Leadership: Dominating with 55.0% market share, public payer applications drive primary demand through automated network management for government healthcare programs, Medicare systems, and public health operations. Specialized systems for public health administration, regulatory compliance, and government healthcare management that exceed administrative standards while maintaining operational efficiency capture significant premiums from government agencies and public health authorities. Opportunity: USD 14.8-17.4 billion.
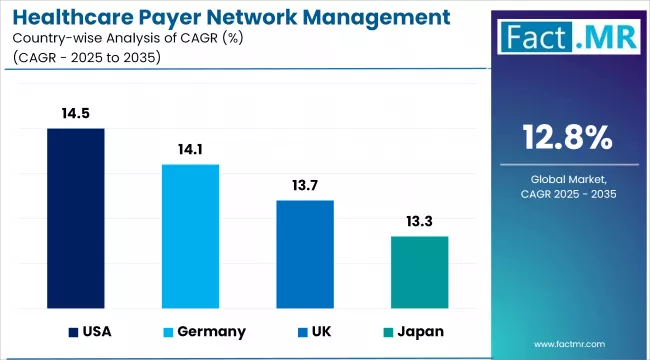
- Pathway C - Regional Market Acceleration: United States (14.5% CAGR) and Germany (14.1% CAGR) lead global growth through aggressive healthcare digitization programs, government healthcare initiatives, and regulatory compliance development. Local partnerships enabling compliance with domestic healthcare regulations, administrative standards, and cost-effective solutions tailored for regional market price points capture expanding demand. Geographic expansion upside: USD 9.2-12.8 billion.
- Pathway D - Cloud-based & Private Payers Applications: Beyond traditional public payer systems, management applications in cloud-based deployments, private insurance, and specialized healthcare operations represent high-growth segments. Advanced management systems for private insurers, cloud platforms, and specialized healthcare requirements that improve efficiency while ensuring regulatory compliance create differentiated value propositions with premium pricing potential. Revenue opportunity: USD 8.5-12.1 billion.
- Pathway E - Technology Integration & Automation: Healthcare automation acceleration drives demand for intelligent management systems, enabling predictive analytics, AI monitoring, and automated compliance management. Advanced solutions supporting Healthcare 4.0, remote monitoring, and predictive analytics expand addressable markets beyond traditional payer applications. Technology advancement pool: USD 7.2-10.8 billion.
- Pathway F - Services & Implementation Solutions: Growing demand for professional services enabling comprehensive deployment across multiple healthcare locations, implementation support, and specialized consulting scenarios. Service solutions supporting operational flexibility, reduced implementation complexity, and multi-site deployment create new market opportunities with moderate premium potential. Services opportunity: USD 6.4-9.6 billion.
- Pathway G - Regulatory Compliance & Data Management: Increasing healthcare regulations drive demand for compliant management systems with data security, privacy protection, and regulatory compliance capabilities. Compliance technology solutions supporting regulatory goals, data protection compliance, and operational cost reduction expand addressable markets with regulatory premium positioning. Compliance solutions pool: USD 5.8-8.4 billion.
Segmental Analysis
The market segments by component into Software and Services categories, representing the evolution from traditional service solutions to comprehensive digital systems for healthcare payer network coverage.
The payer type segmentation divides the market into Public Payers and Private Payers sectors, reflecting distinct requirements for government healthcare programs, private insurance operations, and specialized administrative applications.
The deployment segmentation covers Cloud-based and On-premises categories, with developed markets leading adoption while emerging economies show accelerating growth patterns driven by healthcare digitization programs.
The segmentation structure reveals technology progression from traditional on-premises management systems toward integrated cloud-based platforms with enhanced flexibility and monitoring capabilities, while application diversity spans from public payer administration to comprehensive healthcare management solutions requiring precise automated assistance.
By Component, the Software Segment Accounts for Dominant Market Share
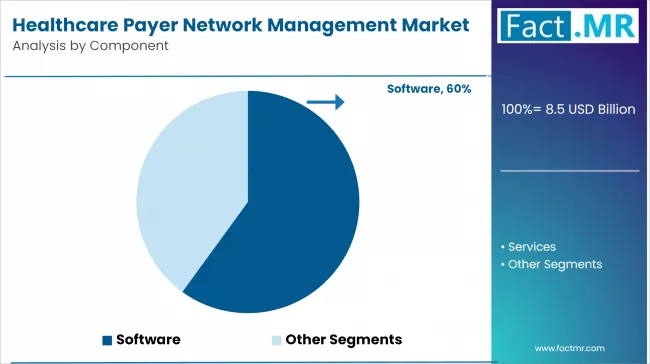
Software solutions command the leading position in the healthcare payer network management market with approximately 60.0% market share through advanced healthcare management features, including high processing capacity, consistent performance, and comprehensive network capabilities that enable healthcare organizations to deploy automated management across diverse payer environments without significant operational modifications.
The segment benefits from healthcare payer preference for high-capacity management systems that provide reliable administrative results without requiring extensive service infrastructure or specialized maintenance protocols. Software system design features enable deployment in major insurance companies, healthcare facilities, and high-volume operations where network consistency and processing efficiency represent critical operational requirements.
Software systems differentiate through established administrative efficiency, proven processing capabilities, and integration with existing healthcare workflows that enhance network effectiveness while maintaining cost-effective operational profiles suitable for healthcare payers of all sizes.
- Advanced network optimization algorithms with established efficiency capabilities and validated performance parameters
- High-processing resources enabling comprehensive payer management and consistent administrative outcomes
- Integration capabilities with healthcare information systems, payer platforms, and operational monitoring systems for comprehensive network workflows
By Payer Type, the Public Payers Segment Accounts for the Largest Market Share
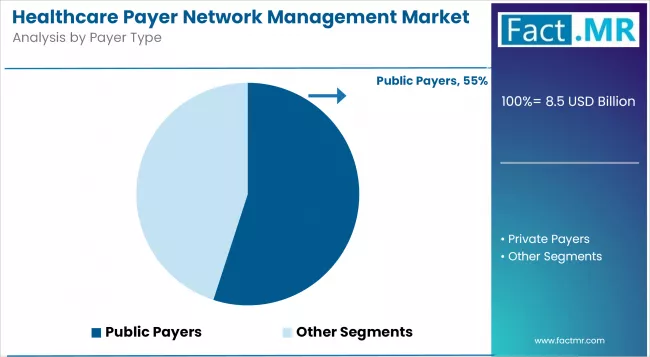
Public payer applications dominate the healthcare payer network management market with approximately 55.0% market share due to widespread adoption of automated network management systems and increasing focus on government healthcare administration, regulatory compliance, and operational efficiency applications that optimize network effectiveness while maintaining administrative consistency.
Public payer customers prioritize system reliability, regulatory compliance, and integration with existing government infrastructure that enables coordinated network management across multiple healthcare types and service lines. The segment benefits from substantial government healthcare budgets and modernization programs that emphasize automated administrative tool acquisition for improved service quality and operational efficiency.
Government healthcare modernization programs incorporate automated network management systems as standard equipment for public health administration and regulatory compliance applications. At the same time, increasing regulatory standards are driving demand for management capabilities that maintain compliance requirements and minimize administrative disruptions.
- Strong growth in government agencies requiring comprehensive automated network assistance capabilities
- Increasing adoption in public health authorities for high-compliance service support applications
- Rising integration with healthcare management platforms for automated network scheduling and quality monitoring
What are the Drivers, Restraints, and Key Trends of the Healthcare Payer Network Management Market?
Healthcare digitization drives primary adoption as payer management systems provide administrative assistance capabilities that enable consistent network operations without manual dependency risks, supporting operational decision-making and compliance missions that require precise network management.
The demand for administrative modernization accelerates market expansion as healthcare payers seek effective network enhancement tools that minimize administrative errors while maintaining operational effectiveness during complex healthcare procedures and provider management scenarios.
Healthcare spending increases worldwide, creating sustained demand for automated network systems that complement traditional administrative equipment and provide operational flexibility in complex healthcare environments.
Capital investment challenges vary across payers regarding the deployment of automated management systems and healthcare budget allocation protocols, which may limit operational flexibility and market penetration in regions with constrained healthcare budgets.
Technical performance limitations persist regarding system adaptability and integration complexity that may reduce effectiveness with legacy healthcare equipment, non-standardized provider formats, or complex administrative workflows that limit network capabilities.
Market fragmentation across multiple healthcare standards and operational requirements creates compatibility concerns between different management system providers and existing healthcare infrastructure.
Adoption accelerates in healthcare and insurance sectors where administrative efficiency justifies system costs, with geographic concentration in developed markets transitioning toward mainstream adoption in emerging economies driven by healthcare digitization and administrative infrastructure development.
Technology development focuses on enhanced network efficiency, improved automation capabilities, and compatibility with diverse healthcare systems that optimize administrative workflow and operational effectiveness. The market could face disruption if alternative healthcare technologies or budget restrictions significantly limit automated management deployment in healthcare or insurance applications.
Analysis of the Healthcare Payer Network Management Market by Key Country
The healthcare payer network management market demonstrates varied regional dynamics with Growth leaders including United States (14.5% CAGR) and Germany (14.1% CAGR) are driving expansion through healthcare digitization and administrative infrastructure development.
Steady performers encompass U.K. (13.7% CAGR), Japan (13.3% CAGR), and South Korea (12.9% CAGR), benefiting from established healthcare industries and advanced administrative automation adoption. Emerging markets feature France (12.5% CAGR), where specialized healthcare applications and administrative technology integration support consistent growth patterns.
| Country | CAGR (2025-2035) |
|---|---|
| United States | 14.5% |
| Germany | 14.1% |
| U.K. | 13.7% |
| Japan | 13.3% |
| South Korea | 12.9% |
| France | 12.5% |
Regional synthesis reveals North American markets leading growth through healthcare digitization and administrative infrastructure development, while European countries maintain steady expansion supported by healthcare technology advancement and EU healthcare standardization requirements. Asian markets show moderate growth driven by healthcare applications and administrative technology integration trends.
United States Drives Global Market Leadership
United States establishes market leadership through aggressive healthcare digitization programs and comprehensive administrative infrastructure development, integrating advanced payer network management systems as standard components in insurance operations and healthcare administration.
The country's 14.5% CAGR through 2035 reflects government initiatives promoting healthcare automation and domestic administrative capabilities that mandate advanced management systems in healthcare facility installations. Growth concentrates in major healthcare hubs, including California, Texas, and New York, where healthcare technology development showcases integrated management systems that appeal to domestic healthcare payers seeking advanced administrative capabilities and operational enhancement applications.
American manufacturers are developing cost-effective payer management solutions that combine domestic production advantages with advanced features, including precision network algorithms and comprehensive healthcare capabilities. Distribution channels through healthcare procurement and administrative equipment suppliers expand market access, while government funding for healthcare technology development supports adoption across diverse insurance and healthcare segments.
- Healthcare systems leading adoption with 91% deployment rate in insurance and government healthcare administrative departments
- Government healthcare programs providing substantial funding for domestic administrative automation development
- Local providers capturing 78% market share through competitive pricing and localized healthcare support
- Insurance segment growth driven by payer requirements for automated administrative systems
- Market development for cost-effective management solutions targeting emerging healthcare markets
Germany Emerges as Technology Innovation Leader
In Berlin, Munich, and Hamburg, healthcare authorities and insurance operators are implementing advanced payer network management systems as standard equipment for healthcare administration and network management applications, driven by increasing healthcare spending and modernization programs that emphasize the use of automated administrative capabilities.
The market is projected to demonstrate a 14.1% CAGR through 2035, supported by government healthcare initiatives and administrative infrastructure development programs that promote the use of advanced management tools for healthcare payers and insurance authorities. German healthcare operators are adopting management systems that provide superior administrative capabilities and network enhancement features, particularly appealing in healthcare regions where service continuity represents critical operational requirements.
Market expansion benefits from growing healthcare technology capabilities and EU technology transfer agreements that enable domestic development of advanced administrative systems for healthcare and insurance applications. Technology adoption follows patterns established in healthcare infrastructure, where operational efficiency and service quality drive procurement decisions and system deployment.
- Healthcare and insurance operator segments are driving initial adoption with 56% annual growth in management system procurement
- Healthcare modernization programs emphasizing automated administrative tools for network management and service quality
- Local healthcare technology companies partnering with international providers for system development
- Healthcare and insurance services implementing management systems for administrative assistance and operational management
United Kingdom Maintains Technology Leadership
U.K.'s advanced healthcare technology market demonstrates sophisticated payer management deployment with documented administrative effectiveness in healthcare departments and insurance centers through integration with existing healthcare systems and administrative infrastructure.
The country leverages healthcare expertise in administrative technology and healthcare systems integration to maintain a 13.7% CAGR through 2035. Healthcare centers, including London, Manchester, and Birmingham, showcase premium installations where payer management integrates with comprehensive healthcare information systems and administrative platforms to optimize network accuracy and operational workflow effectiveness.
British healthcare technology providers prioritize system reliability and NHS regulatory compliance in payer management development, creating demand for premium systems with advanced features, including administrative validation and integration with British healthcare standards. The market benefits from established healthcare industry infrastructure and a willingness to invest in advanced administrative technologies that provide long-term operational benefits and compliance with healthcare regulations.
- Healthcare focuses on NHS standards and system integration, driving premium healthcare segment growth
- Healthcare technology partnerships providing 45% faster administrative validation cycles
- Technology collaboration between British healthcare equipment manufacturers and international healthcare companies
- Healthcare training programs are expanding management integration in administrative management and operational scenarios
Japan Demonstrates Healthcare Excellence
Japan demonstrates steady market development with a 13.3% CAGR through 2035, distinguished by healthcare payers' preference for high-quality management systems that integrate seamlessly with existing healthcare equipment and provide reliable long-term operation in specialized administrative applications.
The market prioritizes advanced features, including precision network algorithms, administrative validation, and integration with comprehensive healthcare platforms that reflect Japanese healthcare expectations for technological sophistication and operational excellence.
South Korea Drives Healthcare Technology Integration
In Seoul, Busan, and other healthcare centers, Korean healthcare operators and insurance authorities are implementing advanced payer network management systems to enhance administrative capabilities and support operational decision-making that aligns with Korean healthcare standards and administrative regulations.
The South Korea market is expected to demonstrate sustained growth with a 12.9% CAGR through 2035, driven by healthcare modernization programs and administrative equipment upgrades that emphasize advanced management tools for healthcare and insurance applications. Korean healthcare facilities are prioritizing management systems that provide superior administrative capabilities while maintaining compliance with healthcare regulations and minimizing operational risks, particularly important in public health and specialized healthcare applications.
Market expansion benefits from healthcare procurement programs that support automated administrative capabilities in healthcare equipment specifications, creating sustained demand across South Korea's healthcare sectors where operational effectiveness and regulatory compliance represent critical requirements. The regulatory framework supports management adoption through healthcare device standards and administrative technology requirements that promote advanced management systems aligned with national healthcare capabilities.
- Healthcare and insurance systems are leading the adoption with administrative equipment modernization programs requiring automated management systems
- Government healthcare procurement providing regulatory support for advanced management system acquisition
- Korean compatibility requirements are driving demand for standardized systems with national healthcare interoperability
- Specialized healthcare departments adopting comprehensive administrative solutions for management automation and operational management
France Shows Strong Regional Leadership
France's market expansion benefits from diverse healthcare demand, including healthcare modernization in Paris and Lyon, insurance system upgrades, and government healthcare programs that increasingly incorporate automated administrative solutions for healthcare management applications. The country maintains a 12.5% CAGR through 2035, driven by rising healthcare awareness and increasing adoption of payer management benefits, including superior administrative capabilities and reduced operational costs.
Market dynamics focus on cost-effective management solutions that balance advanced administrative features with affordability considerations important to French healthcare payers. Growing healthcare infrastructure creates sustained demand for modern administrative systems in new healthcare facilities and administrative equipment modernization projects.
- Healthcare and insurance segments leading growth with focus on administrative automation and service quality applications
- Regional healthcare requirements are driving a diverse product portfolio from basic administration to advanced management platforms
- Local development partnerships with international healthcare technology manufacturers
- Government healthcare initiatives beginning to influence procurement standards and administrative requirements
Europe Market Split by Country
The Healthcare Payer Network Management market in Europe is projected to grow from USD 2.1 billion in 2025 to USD 6.8 billion by 2035, registering a CAGR of 12.5% over the forecast period. Germany is expected to maintain its leadership position with a 28.9% market share in 2025, rising to 30.2% by 2035, supported by its advanced healthcare technology sector and major healthcare centers, including Berlin and Munich.
The United Kingdom follows with a 21.4% share in 2025, projected to reach 20.8% by 2035, driven by comprehensive healthcare modernization programs and administrative technology development initiatives. France holds a 18.2% share in 2025, expected to increase to 19.5% by 2035 through specialized healthcare applications and regulatory standardization requirements.
Italy commands a 11.9% share in 2025, declining to 11.2% by 2035, while Spain accounts for 8.2% in 2025, increasing to 8.7% by 2035. The Nordic Countries region holds 8.5% in 2025, rising to 9.0% by 2035. BENELUX is anticipated to hold 2.4% in 2025, declining to 0.1% by 2035, while the Rest of Western Europe maintains a stable 0.5% share throughout the forecast period.
Public Payers Dominates Healthcare Payer Network Management Demand in Japan
In Japan, the healthcare payer network management market prioritizes public payers applications, which capture the dominant share of healthcare facility and insurance installations due to their advanced features, including high-reliability capabilities and seamless integration with existing healthcare information technology infrastructure.
Japanese healthcare operators emphasize reliability, administrative accuracy, and long-term operational excellence, creating demand for public payer systems that provide comprehensive management capabilities and adaptive administrative control based on regulatory requirements and healthcare complexity scenarios.
Private Payers applications maintain a secondary market position primarily in specialized applications and private insurance installations where operational requirements meet compliance without government dependency limitations.
- Premium focus on public payer systems with advanced administrative algorithms and high-reliability capabilities
- Integration requirements with existing healthcare information systems and administrative management platforms
- Emphasis on administrative reliability and long-term performance in healthcare applications
Healthcare Technology Providers Lead Payer Network Management Services in South Korea
In South Korea, the market structure favors healthcare IT companies, which maintain dominant positions through comprehensive product portfolios and established healthcare procurement networks supporting both healthcare systems and insurance facilities.
These providers offer integrated solutions combining advanced payer management systems with professional implementation services and ongoing technical support that appeal to Korean healthcare operators seeking reliable automated administrative systems.
Government agencies and insurance companies capture moderate market share by providing specialized service capabilities and competitive pricing for standard healthcare installations. At the same time, other providers focus on specialized applications and cost-effective solutions tailored to Korean healthcare characteristics.
- Healthcare IT companies maintaining premium market positioning through advanced administrative offerings
- Government agency networks expanding to support growing demand for professional implementation and administrative support
- System integration capabilities are becoming a key differentiator for healthcare and insurance applications
Competitive Landscape of the Healthcare Payer Network Management Market
The healthcare payer network management market operates with moderate concentration, featuring approximately 20-25 meaningful participants, where leading companies control roughly 65-70% of the global market share through established healthcare technology relationships and comprehensive administrative system portfolios. Competition emphasizes advanced management capabilities, system reliability, and integration with healthcare platforms rather than price-based rivalry.
Market leaders encompass Optum Inc., Anthem Inc., Humana Inc., Aetna Inc., and Cigna Corporation, which maintain competitive advantages through extensive healthcare technology expertise, global healthcare contractor networks, and comprehensive system integration capabilities that create customer switching costs and support premium pricing. These companies leverage decades of healthcare technology experience and ongoing research investments to develop advanced payer management systems with precision administrative algorithms and healthcare validation features.
Technology challengers include McKesson Corporation, Change Healthcare, Cognizant Technology, Wipro Limited, and Infosys Limited, which compete through specialized healthcare administrative focus and innovative management interfaces that appeal to healthcare customers seeking advanced administrative capabilities and operational flexibility. These companies differentiate through rapid technology development cycles and specialized healthcare application focus.
Regional specialists feature companies that focus on specific geographic markets and specialized applications, including government healthcare systems and integrated administrative platforms. Market dynamics favor participants that combine reliable administrative algorithms with advanced healthcare software, including precision network control and automatic healthcare monitoring capabilities.
Competitive pressure intensifies as traditional healthcare equipment contractors expand into payer management systems. At the same time, specialized healthcare companies challenge established players through innovative administrative solutions and cost-effective platforms targeting specialized healthcare segments.
Key Players in the Healthcare Payer Network Management Market
- Optum Inc.
- Anthem Inc.
- Humana Inc.
- Aetna Inc.
- Cigna Corporation
- McKesson Corporation
- Change Healthcare
- Cognizant Technology
- Wipro Limited
- Infosys Limited
Scope of the Report
| Item | Value |
|---|---|
| Quantitative Units | USD 8.5 Billion |
| Component | Software, Services |
| Payer Type | Public Payers, Private Payers |
| Deployment | Cloud-based, On-premises |
| Regions Covered | Asia Pacific, North America, Europe, Latin America, Middle East & Africa |
| Countries Covered | United States, Germany, U.K., Japan, South Korea, France, and 25+ additional countries |
| Key Companies Profiled | Optum Inc., Anthem Inc., Humana Inc., Aetna Inc., Cigna Corporation, McKesson Corporation, Change Healthcare, Cognizant Technology, Wipro Limited, Infosys Limited |
| Additional Attributes | Dollar sales by component and payer type categories, regional adoption trends across Asia Pacific, North America, and Europe, competitive landscape with healthcare technology providers and administrative specialists, healthcare payer preferences for administrative efficiency and system reliability, integration with healthcare information systems and administrative workflows, innovations in network algorithms and automated healthcare management, and development of advanced solutions with enhanced processing and monitoring capabilities. |
Healthcare Payer Network Management Market by Segments
-
Component :
- Software
- Services
-
Payer Type :
- Public Payers
- Private Payers
-
Deployment :
- Cloud-based
- On-premises
-
Region :
- Asia Pacific
- China
- Japan
- South Korea
- India
- ASEAN
- Australia & New Zealand
- Rest of Asia Pacific
- North America
- United States
- Canada
- Mexico
- Europe
- Germany
- United Kingdom
- France
- Italy
- Spain
- Nordic Countries
- BENELUX
- Rest of Europe
- Latin America
- Brazil
- Chile
- Rest of Latin America
- Middle East & Africa
- Kingdom of Saudi Arabia
- Other GCC Countries
- Turkey
- South Africa
- Other African Union
- Rest of Middle East & Africa
- Asia Pacific
Table of Content
- Executive Summary
- Global Market Outlook
- Demand-side Trends
- Supply-side Trends
- Technology Roadmap Analysis
- Analysis and Recommendations
- Market Overview
- Market Coverage / Taxonomy
- Market Definition / Scope / Limitations
- Market Background
- Market Dynamics
- Drivers
- Restraints
- Opportunity
- Trends
- Scenario Forecast
- Demand in Optimistic Scenario
- Demand in Likely Scenario
- Demand in Conservative Scenario
- Opportunity Map Analysis
- Product Life Cycle Analysis
- Supply Chain Analysis
- Investment Feasibility Matrix
- Value Chain Analysis
- PESTLE and Porter’s Analysis
- Regulatory Landscape
- Regional Parent Market Outlook
- Production and Consumption Statistics
- Import and Export Statistics
- Market Dynamics
- Global Market Analysis 2020-2024 and Forecast, 2025-2035
- Historical Market Size Value (USD Billion) & Units Analysis, 2020-2024
- Current and Future Market Size Value (USD Billion) & Units Projections, 2025-2035
- Y-o-Y Growth Trend Analysis
- Absolute $ Opportunity Analysis
- Global Market Pricing Analysis 2020-2024 and Forecast 2025-2035
- Global Market Analysis 2020-2024 and Forecast 2025-2035, By Component
- Introduction / Key Findings
- Historical Market Size Value (USD Billion) & Units Analysis By Component, 2020-2024
- Current and Future Market Size Value (USD Billion) & Units Analysis and Forecast By Component, 2025-2035
- Software
- Services
- Y-o-Y Growth Trend Analysis By Component, 2020-2024
- Absolute $ Opportunity Analysis By Component, 2025-2035
- Global Market Analysis 2020-2024 and Forecast 2025-2035, By Payer Type
- Introduction / Key Findings
- Historical Market Size Value (USD Billion) & Units Analysis By Payer Type, 2020-2024
- Current and Future Market Size Value (USD Billion) & Units Analysis and Forecast By Payer Type, 2025-2035
- Public Payers
- Private Payers
- Y-o-Y Growth Trend Analysis By Payer Type, 2020-2024
- Absolute $ Opportunity Analysis By Payer Type, 2025-2035
- Global Market Analysis 2020-2024 and Forecast 2025-2035, By Deployment
- Introduction / Key Findings
- Historical Market Size Value (USD Billion) & Units Analysis By Deployment, 2020-2024
- Current and Future Market Size Value (USD Billion) & Units Analysis and Forecast By Deployment, 2025-2035
- Cloud-based
- On-premises
- Y-o-Y Growth Trend Analysis By Deployment, 2020-2024
- Absolute $ Opportunity Analysis By Deployment, 2025-2035
- Global Market Analysis 2020-2024 and Forecast 2025-2035, By Region
- Introduction
- Historical Market Size Value (USD Billion) & Units Analysis By Region, 2020-2024
- Current Market Size Value (USD Billion) & Units Analysis and Forecast By Region, 2025-2035
- North America
- Latin America
- Western Europe
- Eastern Europe
- East Asia
- South Asia & Pacific
- Middle East & Africa
- Market Attractiveness Analysis By Region
- North America Market Analysis 2020-2024 and Forecast 2025-2035, By Country
- Historical Market Size Value (USD Billion) & Units Trend Analysis By Market Taxonomy, 2020-2024
- Market Size Value (USD Billion) & Units Forecast By Market Taxonomy, 2025-2035
- By Country
- U.S.
- Canada
- Mexico
- By Component
- By Payer Type
- By Deployment
- By Country
- Market Attractiveness Analysis
- By Country
- By Component
- By Payer Type
- By Deployment
- Key Takeaways
- Latin America Market Analysis 2020-2024 and Forecast 2025-2035, By Country
- Historical Market Size Value (USD Billion) & Units Trend Analysis By Market Taxonomy, 2020-2024
- Market Size Value (USD Billion) & Units Forecast By Market Taxonomy, 2025-2035
- By Country
- Brazil
- Chile
- Rest of Latin America
- By Component
- By Payer Type
- By Deployment
- By Country
- Market Attractiveness Analysis
- By Country
- By Component
- By Payer Type
- By Deployment
- Key Takeaways
- Western Europe Market Analysis 2020-2024 and Forecast 2025-2035, By Country
- Historical Market Size Value (USD Billion) & Units Trend Analysis By Market Taxonomy, 2020-2024
- Market Size Value (USD Billion) & Units Forecast By Market Taxonomy, 2025-2035
- By Country
- Germany
- U.K.
- Italy
- Spain
- France
- Nordic
- BENELUX
- Rest of Europe
- By Component
- By Payer Type
- By Deployment
- By Country
- Market Attractiveness Analysis
- By Country
- By Component
- By Payer Type
- By Deployment
- Key Takeaways
- Eastern Europe Market Analysis 2020-2024 and Forecast 2025-2035, By Country
- Historical Market Size Value (USD Billion) & Units Trend Analysis By Market Taxonomy, 2020-2024
- Market Size Value (USD Billion) & Units Forecast By Market Taxonomy, 2025-2035
- By Country
- Russia
- Poland
- Hungary
- Balkan & Baltics
- Rest of Eastern Europe
- By Component
- By Payer Type
- By Deployment
- By Country
- Market Attractiveness Analysis
- By Country
- By Component
- By Payer Type
- By Deployment
- Key Takeaways
- East Asia Market Analysis 2020-2024 and Forecast 2025-2035, By Country
- Historical Market Size Value (USD Billion) & Units Trend Analysis By Market Taxonomy, 2020-2024
- Market Size Value (USD Billion) & Units Forecast By Market Taxonomy, 2025-2035
- By Country
- China
- Japan
- South Korea
- By Component
- By Payer Type
- By Deployment
- By Country
- Market Attractiveness Analysis
- By Country
- By Component
- By Payer Type
- By Deployment
- Key Takeaways
- South Asia & Pacific Market Analysis 2020-2024 and Forecast 2025-2035, By Country
- Historical Market Size Value (USD Billion) & Units Trend Analysis By Market Taxonomy, 2020-2024
- Market Size Value (USD Billion) & Units Forecast By Market Taxonomy, 2025-2035
- By Country
- India
- ASEAN
- Australia & New Zealand
- Rest of South Asia & Pacific
- By Component
- By Payer Type
- By Deployment
- By Country
- Market Attractiveness Analysis
- By Country
- By Component
- By Payer Type
- By Deployment
- Key Takeaways
- Middle East & Africa Market Analysis 2020-2024 and Forecast 2025-2035, By Country
- Historical Market Size Value (USD Billion) & Units Trend Analysis By Market Taxonomy, 2020-2024
- Market Size Value (USD Billion) & Units Forecast By Market Taxonomy, 2025-2035
- By Country
- Kingdom of Saudi Arabia
- Other GCC Countries
- Turkiye
- South Africa
- Other African Union
- Rest of Middle East & Africa
- By Component
- By Payer Type
- By Deployment
- By Country
- Market Attractiveness Analysis
- By Country
- By Component
- By Payer Type
- By Deployment
- Key Takeaways
- Key Countries Market Analysis
- U.S.
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Canada
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Mexico
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Brazil
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Chile
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Germany
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- U.K.
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Italy
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Spain
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- France
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Nordic
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- BENELUX
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Russia
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Poland
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Hungary
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Balkan & Baltics
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- China
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Japan
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- South Korea
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- India
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- ASEAN
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Australia & New Zealand
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Kingdom of Saudi Arabia
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- Turkiye
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- South Africa
- Pricing Analysis
- Market Share Analysis, 2024
- By Component
- By Payer Type
- By Deployment
- U.S.
- Market Structure Analysis
- Competition Dashboard
- Competition Benchmarking
- Market Share Analysis of Top Players
- By Regional
- By Component
- By Payer Type
- By Deployment
- Competition Analysis
- Competition Deep Dive
- Optum Inc.
- Overview
- Product Portfolio
- Profitability by Market Segments (Product/Age /Sales Channel/Region)
- Sales Footprint
- Strategy Overview
- Anthem Inc.
- Humana Inc.
- Aetna Inc.
- Cigna Corporation
- McKesson Corporation
- Change Healthcare
- Cognizant Technology
- Wipro Limited
- Infosys Limited
- Optum Inc.
- Competition Deep Dive
- Assumptions & Acronyms Used
- Research Methodology
List Of Table
- Table 1: Global Market Value (USD Billion) Forecast by Region, 2020 to 2035
- Table 2: Global Market Units Forecast by Region, 2020 to 2035
- Table 3: Global Market Value (USD Billion) Forecast by Component, 2020 to 2035
- Table 4: Global Market Units Forecast by Component, 2020 to 2035
- Table 5: Global Market Value (USD Billion) Forecast by Payer Type, 2020 to 2035
- Table 6: Global Market Units Forecast by Payer Type, 2020 to 2035
- Table 7: Global Market Value (USD Billion) Forecast by Deployment, 2020 to 2035
- Table 8: Global Market Units Forecast by Deployment, 2020 to 2035
- Table 9: North America Market Value (USD Billion) Forecast by Country, 2020 to 2035
- Table 10: North America Market Units Forecast by Country, 2020 to 2035
- Table 11: North America Market Value (USD Billion) Forecast by Component, 2020 to 2035
- Table 12: North America Market Units Forecast by Component, 2020 to 2035
- Table 13: North America Market Value (USD Billion) Forecast by Payer Type, 2020 to 2035
- Table 14: North America Market Units Forecast by Payer Type, 2020 to 2035
- Table 15: North America Market Value (USD Billion) Forecast by Deployment, 2020 to 2035
- Table 16: North America Market Units Forecast by Deployment, 2020 to 2035
- Table 17: Latin America Market Value (USD Billion) Forecast by Country, 2020 to 2035
- Table 18: Latin America Market Units Forecast by Country, 2020 to 2035
- Table 19: Latin America Market Value (USD Billion) Forecast by Component, 2020 to 2035
- Table 20: Latin America Market Units Forecast by Component, 2020 to 2035
- Table 21: Latin America Market Value (USD Billion) Forecast by Payer Type, 2020 to 2035
- Table 22: Latin America Market Units Forecast by Payer Type, 2020 to 2035
- Table 23: Latin America Market Value (USD Billion) Forecast by Deployment, 2020 to 2035
- Table 24: Latin America Market Units Forecast by Deployment, 2020 to 2035
- Table 25: Western Europe Market Value (USD Billion) Forecast by Country, 2020 to 2035
- Table 26: Western Europe Market Units Forecast by Country, 2020 to 2035
- Table 27: Western Europe Market Value (USD Billion) Forecast by Component, 2020 to 2035
- Table 28: Western Europe Market Units Forecast by Component, 2020 to 2035
- Table 29: Western Europe Market Value (USD Billion) Forecast by Payer Type, 2020 to 2035
- Table 30: Western Europe Market Units Forecast by Payer Type, 2020 to 2035
- Table 31: Western Europe Market Value (USD Billion) Forecast by Deployment, 2020 to 2035
- Table 32: Western Europe Market Units Forecast by Deployment, 2020 to 2035
- Table 33: Eastern Europe Market Value (USD Billion) Forecast by Country, 2020 to 2035
- Table 34: Eastern Europe Market Units Forecast by Country, 2020 to 2035
- Table 35: Eastern Europe Market Value (USD Billion) Forecast by Component, 2020 to 2035
- Table 36: Eastern Europe Market Units Forecast by Component, 2020 to 2035
- Table 37: Eastern Europe Market Value (USD Billion) Forecast by Payer Type, 2020 to 2035
- Table 38: Eastern Europe Market Units Forecast by Payer Type, 2020 to 2035
- Table 39: Eastern Europe Market Value (USD Billion) Forecast by Deployment, 2020 to 2035
- Table 40: Eastern Europe Market Units Forecast by Deployment, 2020 to 2035
- Table 41: East Asia Market Value (USD Billion) Forecast by Country, 2020 to 2035
- Table 42: East Asia Market Units Forecast by Country, 2020 to 2035
- Table 43: East Asia Market Value (USD Billion) Forecast by Component, 2020 to 2035
- Table 44: East Asia Market Units Forecast by Component, 2020 to 2035
- Table 45: East Asia Market Value (USD Billion) Forecast by Payer Type, 2020 to 2035
- Table 46: East Asia Market Units Forecast by Payer Type, 2020 to 2035
- Table 47: East Asia Market Value (USD Billion) Forecast by Deployment, 2020 to 2035
- Table 48: East Asia Market Units Forecast by Deployment, 2020 to 2035
- Table 49: South Asia & Pacific Market Value (USD Billion) Forecast by Country, 2020 to 2035
- Table 50: South Asia & Pacific Market Units Forecast by Country, 2020 to 2035
- Table 51: South Asia & Pacific Market Value (USD Billion) Forecast by Component, 2020 to 2035
- Table 52: South Asia & Pacific Market Units Forecast by Component, 2020 to 2035
- Table 53: South Asia & Pacific Market Value (USD Billion) Forecast by Payer Type, 2020 to 2035
- Table 54: South Asia & Pacific Market Units Forecast by Payer Type, 2020 to 2035
- Table 55: South Asia & Pacific Market Value (USD Billion) Forecast by Deployment, 2020 to 2035
- Table 56: South Asia & Pacific Market Units Forecast by Deployment, 2020 to 2035
- Table 57: Middle East & Africa Market Value (USD Billion) Forecast by Country, 2020 to 2035
- Table 58: Middle East & Africa Market Units Forecast by Country, 2020 to 2035
- Table 59: Middle East & Africa Market Value (USD Billion) Forecast by Component, 2020 to 2035
- Table 60: Middle East & Africa Market Units Forecast by Component, 2020 to 2035
- Table 61: Middle East & Africa Market Value (USD Billion) Forecast by Payer Type, 2020 to 2035
- Table 62: Middle East & Africa Market Units Forecast by Payer Type, 2020 to 2035
- Table 63: Middle East & Africa Market Value (USD Billion) Forecast by Deployment, 2020 to 2035
- Table 64: Middle East & Africa Market Units Forecast by Deployment, 2020 to 2035
List Of Figures
- Figure 1: Global Market Units Forecast 2020 to 2035
- Figure 2: Global Market Pricing Analysis
- Figure 3: Global Market Value (USD Billion) Forecast 2020 to 2035
- Figure 4: Global Market Value Share and BPS Analysis by Component, 2025 and 2035
- Figure 5: Global Market Y-o-Y Growth Comparison by Component, 2025 to 2035
- Figure 6: Global Market Attractiveness Analysis by Component
- Figure 7: Global Market Value Share and BPS Analysis by Payer Type, 2025 and 2035
- Figure 8: Global Market Y-o-Y Growth Comparison by Payer Type, 2025 to 2035
- Figure 9: Global Market Attractiveness Analysis by Payer Type
- Figure 10: Global Market Value Share and BPS Analysis by Deployment, 2025 and 2035
- Figure 11: Global Market Y-o-Y Growth Comparison by Deployment, 2025 to 2035
- Figure 12: Global Market Attractiveness Analysis by Deployment
- Figure 13: Global Market Value (USD Billion) Share and BPS Analysis by Region, 2025 and 2035
- Figure 14: Global Market Y-o-Y Growth Comparison by Region, 2025 to 2035
- Figure 15: Global Market Attractiveness Analysis by Region
- Figure 16: North America Market Incremental $ Opportunity, 2025 to 2035
- Figure 17: Latin America Market Incremental $ Opportunity, 2025 to 2035
- Figure 18: Western Europe Market Incremental $ Opportunity, 2025 to 2035
- Figure 19: Eastern Europe Market Incremental $ Opportunity, 2025 to 2035
- Figure 20: East Asia Market Incremental $ Opportunity, 2025 to 2035
- Figure 21: South Asia & Pacific Market Incremental $ Opportunity, 2025 to 2035
- Figure 22: Middle East & Africa Market Incremental $ Opportunity, 2025 to 2035
- Figure 23: North America Market Value Share and BPS Analysis by Country, 2025 and 2035
- Figure 24: North America Market Value Share and BPS Analysis by Component, 2025 and 2035
- Figure 25: North America Market Y-o-Y Growth Comparison by Component, 2025 to 2035
- Figure 26: North America Market Attractiveness Analysis by Component
- Figure 27: North America Market Value Share and BPS Analysis by Payer Type, 2025 and 2035
- Figure 28: North America Market Y-o-Y Growth Comparison by Payer Type, 2025 to 2035
- Figure 29: North America Market Attractiveness Analysis by Payer Type
- Figure 30: North America Market Value Share and BPS Analysis by Deployment, 2025 and 2035
- Figure 31: North America Market Y-o-Y Growth Comparison by Deployment, 2025 to 2035
- Figure 32: North America Market Attractiveness Analysis by Deployment
- Figure 33: Latin America Market Value Share and BPS Analysis by Country, 2025 and 2035
- Figure 34: Latin America Market Value Share and BPS Analysis by Component, 2025 and 2035
- Figure 35: Latin America Market Y-o-Y Growth Comparison by Component, 2025 to 2035
- Figure 36: Latin America Market Attractiveness Analysis by Component
- Figure 37: Latin America Market Value Share and BPS Analysis by Payer Type, 2025 and 2035
- Figure 38: Latin America Market Y-o-Y Growth Comparison by Payer Type, 2025 to 2035
- Figure 39: Latin America Market Attractiveness Analysis by Payer Type
- Figure 40: Latin America Market Value Share and BPS Analysis by Deployment, 2025 and 2035
- Figure 41: Latin America Market Y-o-Y Growth Comparison by Deployment, 2025 to 2035
- Figure 42: Latin America Market Attractiveness Analysis by Deployment
- Figure 43: Western Europe Market Value Share and BPS Analysis by Country, 2025 and 2035
- Figure 44: Western Europe Market Value Share and BPS Analysis by Component, 2025 and 2035
- Figure 45: Western Europe Market Y-o-Y Growth Comparison by Component, 2025 to 2035
- Figure 46: Western Europe Market Attractiveness Analysis by Component
- Figure 47: Western Europe Market Value Share and BPS Analysis by Payer Type, 2025 and 2035
- Figure 48: Western Europe Market Y-o-Y Growth Comparison by Payer Type, 2025 to 2035
- Figure 49: Western Europe Market Attractiveness Analysis by Payer Type
- Figure 50: Western Europe Market Value Share and BPS Analysis by Deployment, 2025 and 2035
- Figure 51: Western Europe Market Y-o-Y Growth Comparison by Deployment, 2025 to 2035
- Figure 52: Western Europe Market Attractiveness Analysis by Deployment
- Figure 53: Eastern Europe Market Value Share and BPS Analysis by Country, 2025 and 2035
- Figure 54: Eastern Europe Market Value Share and BPS Analysis by Component, 2025 and 2035
- Figure 55: Eastern Europe Market Y-o-Y Growth Comparison by Component, 2025 to 2035
- Figure 56: Eastern Europe Market Attractiveness Analysis by Component
- Figure 57: Eastern Europe Market Value Share and BPS Analysis by Payer Type, 2025 and 2035
- Figure 58: Eastern Europe Market Y-o-Y Growth Comparison by Payer Type, 2025 to 2035
- Figure 59: Eastern Europe Market Attractiveness Analysis by Payer Type
- Figure 60: Eastern Europe Market Value Share and BPS Analysis by Deployment, 2025 and 2035
- Figure 61: Eastern Europe Market Y-o-Y Growth Comparison by Deployment, 2025 to 2035
- Figure 62: Eastern Europe Market Attractiveness Analysis by Deployment
- Figure 63: East Asia Market Value Share and BPS Analysis by Country, 2025 and 2035
- Figure 64: East Asia Market Value Share and BPS Analysis by Component, 2025 and 2035
- Figure 65: East Asia Market Y-o-Y Growth Comparison by Component, 2025 to 2035
- Figure 66: East Asia Market Attractiveness Analysis by Component
- Figure 67: East Asia Market Value Share and BPS Analysis by Payer Type, 2025 and 2035
- Figure 68: East Asia Market Y-o-Y Growth Comparison by Payer Type, 2025 to 2035
- Figure 69: East Asia Market Attractiveness Analysis by Payer Type
- Figure 70: East Asia Market Value Share and BPS Analysis by Deployment, 2025 and 2035
- Figure 71: East Asia Market Y-o-Y Growth Comparison by Deployment, 2025 to 2035
- Figure 72: East Asia Market Attractiveness Analysis by Deployment
- Figure 73: South Asia & Pacific Market Value Share and BPS Analysis by Country, 2025 and 2035
- Figure 74: South Asia & Pacific Market Value Share and BPS Analysis by Component, 2025 and 2035
- Figure 75: South Asia & Pacific Market Y-o-Y Growth Comparison by Component, 2025 to 2035
- Figure 76: South Asia & Pacific Market Attractiveness Analysis by Component
- Figure 77: South Asia & Pacific Market Value Share and BPS Analysis by Payer Type, 2025 and 2035
- Figure 78: South Asia & Pacific Market Y-o-Y Growth Comparison by Payer Type, 2025 to 2035
- Figure 79: South Asia & Pacific Market Attractiveness Analysis by Payer Type
- Figure 80: South Asia & Pacific Market Value Share and BPS Analysis by Deployment, 2025 and 2035
- Figure 81: South Asia & Pacific Market Y-o-Y Growth Comparison by Deployment, 2025 to 2035
- Figure 82: South Asia & Pacific Market Attractiveness Analysis by Deployment
- Figure 83: Middle East & Africa Market Value Share and BPS Analysis by Country, 2025 and 2035
- Figure 84: Middle East & Africa Market Value Share and BPS Analysis by Component, 2025 and 2035
- Figure 85: Middle East & Africa Market Y-o-Y Growth Comparison by Component, 2025 to 2035
- Figure 86: Middle East & Africa Market Attractiveness Analysis by Component
- Figure 87: Middle East & Africa Market Value Share and BPS Analysis by Payer Type, 2025 and 2035
- Figure 88: Middle East & Africa Market Y-o-Y Growth Comparison by Payer Type, 2025 to 2035
- Figure 89: Middle East & Africa Market Attractiveness Analysis by Payer Type
- Figure 90: Middle East & Africa Market Value Share and BPS Analysis by Deployment, 2025 and 2035
- Figure 91: Middle East & Africa Market Y-o-Y Growth Comparison by Deployment, 2025 to 2035
- Figure 92: Middle East & Africa Market Attractiveness Analysis by Deployment
- Figure 93: Global Market - Tier Structure Analysis
- Figure 94: Global Market - Company Share Analysis
- FAQs -
How big is the Healthcare Payer Network Management market in 2025?
The global Healthcare Payer Network Management market is valued at USD 8.5 billion in 2025.
What will be the size of the Healthcare Payer Network Management market in 2035?
The size of the Healthcare Payer Network Management market is projected to reach USD 28.4 billion by 2035.
How much will the Healthcare Payer Network Management market grow between 2025 and 2035?
The Healthcare Payer Network Management market is expected to grow at a 12.8?GR between 2025 and 2035.
What are the key component segments in the Healthcare Payer Network Management market?
The key component segments in the Healthcare Payer Network Management market are Software and Services.
Which payer type segment is expected to contribute a significant share to the Healthcare Payer Network Management market in 2025?
In terms of payer type, the Public Payers segment is set to command the dominant share in the Healthcare Payer Network Management market in 2025.